Understanding Titanium Plates and Their Properties
Titanium plates have emerged as a game-changer in orthopedic surgery, offering unparalleled advantages in bone fracture treatment. These medical devices are crafted from high-quality titanium alloys, typically Ti6Al4V ELI (Extra Low Interstitial), known for its exceptional biocompatibility and mechanical properties. The allure of titanium in medical applications stems from its unique combination of strength and lightweight nature. A titanium plate for bone fracture exhibits remarkable tensile strength, surpassing that of many other metals used in medical implants. This strength allows the plate to withstand the considerable forces exerted on bones during daily activities, ensuring stability throughout the healing process.
Moreover, titanium's low density translates to a lightweight implant that doesn't burden the patient with unnecessary weight. This characteristic is particularly beneficial for patients recovering from fractures in weight-bearing bones, as it minimizes the risk of implant-related discomfort or fatigue. Maybe the most significant property of titanium plates is their biocompatibility. The human body for the most part acknowledges titanium inserts without unfavorable responses, decreasing the chance of dismissal or irritation. This acknowledgment is mostly due to titanium's capacity to frame a steady oxide layer on its surface, which acts as a defensive boundary between the embed and encompassing tissues.
Furthermore, titanium exhibits osseointegration properties, meaning it can form a strong bond with bone tissue. This integration enhances the stability of the fracture fixation and promotes faster healing. As the bone heals, it grows around and into the microscopic pores on the titanium plate's surface, creating a robust and durable connection. The corrosion resistance of titanium is another factor that makes it an ideal choice for long-term implants. Unlike some other metals, titanium doesn't degrade significantly over time when exposed to bodily fluids, ensuring the longevity and reliability of the implant.
The Application Process of Titanium Plates in Fracture Treatment
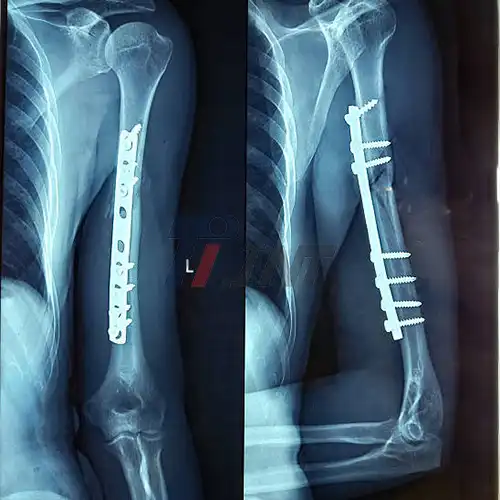
The use of a titanium plate for bone fracture is a sophisticated medical procedure that requires precision and expertise. The process begins with a thorough assessment of the fracture, including imaging studies such as X-rays, CT scans, or MRIs to determine the exact nature and location of the break. Once the fracture is fully understood, the surgeon selects the appropriate titanium plate. These plates come in various shapes and sizes, each designed for specific types of fractures and anatomical locations. For instance, a plate used for a femur fracture will differ significantly from one used for a wrist fracture.
The surgical procedure, known as open reduction and internal fixation (ORIF), involves making an incision to access the fractured bone. The surgeon then carefully aligns the broken bone fragments, a process called reduction. This step is crucial as proper alignment is essential for optimal healing and restoration of function. With the bone fragments aligned, the titanium plate is positioned across the fracture site. The plate is secured to the bone using titanium screws, which are drilled into pre-determined holes in the plate. These screws, also made of biocompatible titanium, work in tandem with the plate to provide stable fixation of the fracture.
In some cases, additional techniques may be employed alongside the titanium plate. For instance, bone grafts might be used to promote healing in complex fractures or in cases where there's significant bone loss. These grafts can be sourced from the patient's own body (autograft) or from a donor (allograft). The placement of the titanium plate for bone fracture requires meticulous attention to detail. The surgeon must ensure that the plate doesn't interfere with surrounding tissues, blood vessels, or nerves. They must also consider the biomechanics of the bone and joint to ensure that the plate provides stability without restricting normal movement.
After the plate is safely input, the surgical location is completely cleaned and closed. Post-operative care ordinarily includes a period of immobilization taken after by a carefully organized restoration program. This program is planned to advance recuperation, reestablish the run of movement, and steadily increment weight-bearing on the affected appendage.
Long-Term Implications and Benefits of Titanium Plates
The use of a titanium plate for bone fracture offers numerous long-term benefits that contribute to improved patient outcomes and quality of life. Understanding these implications is crucial for patients and healthcare providers alike. One of the essential focal points of titanium plates is their toughness. Not at all like a few other materials utilized in orthopedic inserts, titanium plates can stay in the body uncertainly without debasement or misfortune of work. This life span disposes of the requirement for amendment surgeries in most cases, diminishing the hazard of complications and the budgetary burden on patients.
The biocompatibility of titanium also plays a significant role in long-term outcomes. The low risk of allergic reactions or rejection means that patients are less likely to experience chronic inflammation or other immune-related complications. This factor is particularly important for individuals with metal sensitivities or autoimmune conditions.
Another long-term advantage is the conservation of bone thickness. Conventional strategies to break obsession, such as casting, can lead to bone misfortune due to drawn-out immobilization. Titanium plates, in any case, permit prior mobilization and weight-bearing, which makes a difference in keeping up bone thickness and muscle quality. This advantage is particularly significant for more seasoned patients or those at hazard of osteoporosis.
The stability provided by titanium plates also contributes to improved functional outcomes. By ensuring proper alignment throughout the healing process, these implants help prevent malunion or non-union of fractures. This stability translates to better joint function, reduced risk of arthritis, and improved overall mobility in the long term.
It's vital to note that whereas titanium plates offer various benefits, they are not without potential disadvantages. A few patients may experience distress or cold affectability around the embed location, especially in regions with lean delicate tissue scope. In uncommon cases, the plates may require to be expelled due to the bothering of encompassing tissues or obstructions with joint versatility.
Conclusion
The role of titanium plate for bone fracture recovery is undeniably significant. These innovative medical devices have transformed the landscape of orthopedic surgery, offering a blend of strength, biocompatibility, and longevity that is unmatched by other materials. From their unique properties to their application process and long-term implications, titanium plates have proven to be invaluable tools in the treatment of complex fractures.
For those interested in learning more about medical titanium products, including titanium plates for bone fractures, Baoji INT Medical Titanium Co., Ltd. offers a wealth of expertise and high-quality products. With over 30 years of experience in the research, development, and production of titanium materials, INT stands at the forefront of the medical titanium industry. For more information or inquiries, don't hesitate to reach out to them at export@tiint.com.










 2025-09-04 09:10:37
2025-09-04 09:10:37
_1753427753918.webp)





