The Evolution of Maxillofacial Surgery and Titanium Plates
Maxillofacial surgery has come a long way since its beginning. The field has seen surprising progressions in methods, materials, and advances, all pointed at moving forward persistent care and surgical results. One of the most noteworthy breakthroughs in this space has been the presentation and broad selection of titanium plates for maxillofacial remaking.
Historical Perspective on Maxillofacial Reconstruction
In the early days of maxillofacial surgery, reconstruction techniques were limited and often yielded suboptimal results. Surgeons relied on rudimentary materials such as wire fixation and non-biocompatible metals, which frequently led to complications and poor aesthetic outcomes. The search for better solutions was driven by the need to address complex facial injuries resulting from wars, accidents, and diseases.
The Advent of Titanium in Maxillofacial Surgery
The presentation of titanium in maxillofacial surgery stamped a turning point in the field. Titanium's special properties, counting its fabulous biocompatibility, tall strength-to-weight proportion, and erosion resistance, made it an perfect fabric for inserts and obsession gadgets. The advancement of titanium plates particularly planned for maxillofacial remaking opened up modern conceivable outcomes for specialists to accomplish superior utilitarian and stylish comes about.
Advancements in Titanium Plate Design and Manufacturing
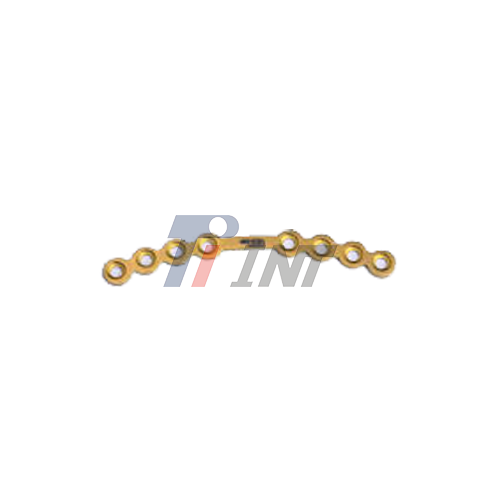
Over a long time, maxillofacial surgery titanium plates have experienced critical changes in plan and fabricating forms. Advanced titanium plates are accessible in different shapes, sizes, and thicknesses to oblige diverse anatomical prerequisites. Progressed fabricating strategies, such as 3D printing and computer-aided planning, have empowered the generation of patient-specific inserts, advancing improving surgical exactness and results.
The Advantages of Titanium Plates in Maxillofacial Reconstruction
Titanium plates have become the gold standard in maxillofacial reconstruction due to their numerous advantages over traditional materials. These benefits have significantly contributed to improved surgical outcomes and patient satisfaction.
Biocompatibility and Long-term Safety
One of the most basic qualities of titanium plates is their excellent biocompatibility. Titanium is well-tolerated by the human body, minimizing the chance of antagonistic responses or dismissal. This property makes titanium plates secure for long-term implantation, a significant figure in maxillofacial reproduction where inserts regularly require staying in place for amplified periods or indeed forever.
Strength and Durability
Titanium plates offer an exceptional combination of strength and lightweight properties. With a tensile strength of ≥ 830 MPa, these plates provide robust support for bone fragments while maintaining their structural integrity over time. The high strength-to-weight ratio of titanium allows for the use of thinner plates without compromising stability, resulting in less bulky reconstructions and improved patient comfort.
Corrosion Resistance and Long-lasting Performance
The corrosion-resistant nature of titanium ensures that plates maintain their structural integrity even in the demanding environment of the human body. This resistance to degradation contributes to the long-lasting performance of titanium plates, reducing the need for revision surgeries and improving overall patient outcomes.
Customization and Versatility
Maxillofacial surgery titanium plates are highly customizable, available in various sizes and surface treatments to meet different surgical needs. With thicknesses ranging from 0.5mm to 2mm and customizable widths and lengths, surgeons can select the most appropriate plate for each unique case. Additionally, surface treatments such as anodization or sandblasting can be applied to enhance osseointegration or achieve specific aesthetic results.
Fatigue Resistance and Reliability
The excellent fatigue resistance of titanium plates ensures their long-term reliability in maxillofacial reconstruction. This property is particularly important in areas subject to repeated stress, such as the mandible during chewing. The fatigue-resistant nature of titanium plates contributes to reduced rates of hardware failure and the need for revision surgeries.
Clinical Applications and Surgical Techniques
The versatility of titanium plates has expanded the scope of maxillofacial reconstruction, enabling surgeons to address a wide range of clinical scenarios with improved precision and outcomes.
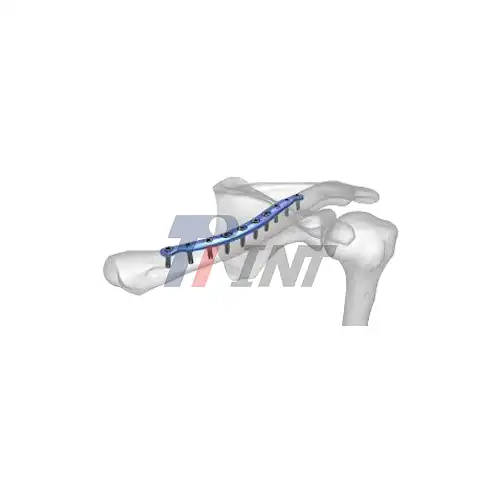
Trauma Reconstruction
In cases of facial trauma, such as fractures resulting from accidents or assaults, maxillofacial surgery titanium plates play a crucial role in restoring facial structure and function. These plates provide stable fixation for fractured bones, allowing for proper healing and alignment. The ability to contour titanium plates to match the patient's unique facial anatomy ensures optimal aesthetic results alongside functional recovery.
Orthognathic Surgery
Titanium plates are extensively used in orthognathic surgery to correct jaw deformities and malocclusions. These procedures often involve repositioning the maxilla or mandible to achieve proper bite alignment and facial harmony. The strength and stability provided by titanium plates are essential for maintaining the new jaw position during the healing process, contributing to successful outcomes in these complex surgeries.
Post-oncologic Reconstruction
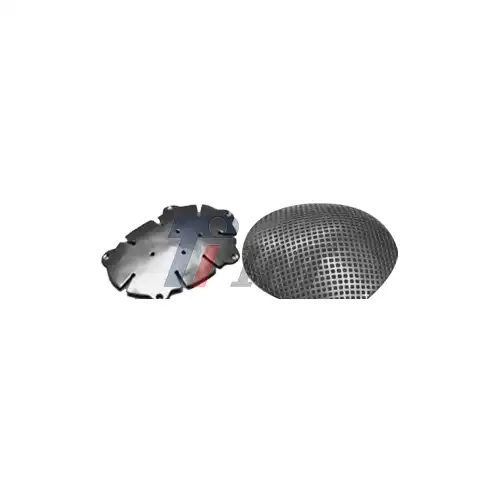
Taking after the evacuation of cancerous tumors in the maxillofacial locale, recreation is regularly vital to reestablish frame and work. Titanium plates serve as a vital instrument in these cases, giving a system for revamping the facial skeleton. When combined with bone units or folds, titanium plates empower specialists to reproduce complex three-dimensional structures, altogether moving forward patients' quality of life after cancer treatment.
Congenital Deformity Correction
Patients with congenital facial deformities, such as cleft lip and palate or craniofacial syndromes, often require extensive reconstruction. Titanium plates offer the flexibility and strength needed to address these challenging cases. The ability to customize plate size and shape allows surgeons to tailor their approach to each patient's unique anatomy, facilitating more precise and aesthetically pleasing outcomes.
Surgical Techniques and Considerations
The successful use of titanium plates in maxillofacial reconstruction relies on proper surgical technique and careful planning. Surgeons must consider factors such as plate placement, screw positioning, and soft tissue management to optimize results. Advanced imaging technologies, such as 3D CT scans and computer-aided surgical planning, have greatly enhanced the precision of these procedures.
Minimally invasive approaches have also been developed to reduce surgical morbidity and improve recovery times. Techniques such as endoscopic-assisted plate placement allow for smaller incisions and reduced soft tissue disruption, particularly beneficial in areas where aesthetics are a primary concern.
Post-operative Care and Follow-up
Whereas titanium plates offer great long-term steadiness, legitimate postoperative care remains significant for ideal results. Patients ordinarily require near follow-up to screen mending, guarantee appropriate impediment, and address any potential complications. In most cases, titanium plates can be cleared out and put in inconclusively, disposing of the need for expulsion surgeries and lessening, by and large, the treatment burden for patients.
Conclusion
The use of maxillofacial surgery titanium plates has transformed the field of oral and maxillofacial surgery, offering patients improved functional and aesthetic outcomes across a wide range of clinical scenarios. The unique properties of titanium, including its biocompatibility, strength, and versatility, have made it an indispensable tool in the surgeon's armamentarium.
For those interested in learning more about medical titanium products, including titanium plates for maxillofacial surgery, Baoji INT Medical Titanium Co., Ltd. offers a comprehensive range of high-quality titanium materials. With over 30 years of experience in the research, development, and production of titanium materials, INT provides cutting-edge technology and expertise in the medical titanium industry. For further information or inquiries, please contact us at export@tiint.com.










 2025-07-04 14:58:13
2025-07-04 14:58:13

_1752462620877.webp)
_1750664157440.webp)
_1749191822714.webp)