The Evolution of Cranioplasty Materials
Cranioplasty has come a long way since its beginning. Early endeavors at repairing cranium absconds included utilizing materials like coconut shells and gold plates. As therapeutic science progressed, so did the materials utilized in this basic method. Nowadays, specialists have plenty of choices at their transfer, extending from autologous bone joints to manufactured materials.
Autologous bone, gathered from the patient's own body, was long considered the gold standard for cranioplasty. Be that as it may, it comes with confinements such as potential resorption and the requirement for extra surgery to collect the bone. This is driven by the investigation of elective materials that might give way better results and decrease understanding distress.
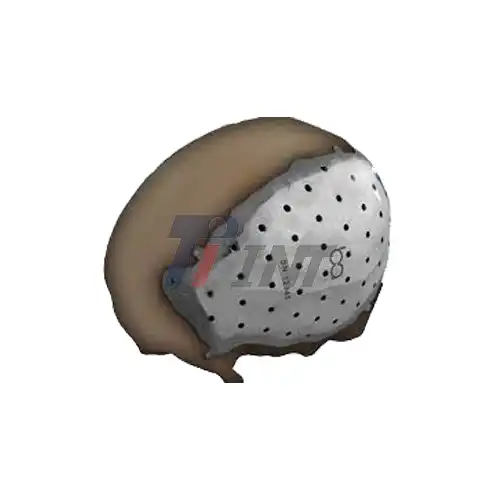
Engineered materials like polymethyl methacrylate (PMMA), hydroxyapatite, and polyetheretherketone (Look) have picked up ubiquity due to their accessibility and ease of use. Be that as it may, each of these materials has its own set of claims and downsides. For occurrence, PMMA is cost-effective but may not coordinate well with the encompassing tissue, whereas hydroxyapatite offers fabulous biocompatibility but needs mechanical quality. Enter titanium - a material that has revolutionized the field of cranioplasty. Titanium plate brain surgery has become increasingly prevalent due to the unique properties of this remarkable metal.
The Titanium Advantage in Cranioplasty
Titanium has emerged as a superior material for cranioplasty, offering a combination of properties that make it ideal for reconstructing the skull. Let's explore the key advantages that have propelled titanium to the forefront of cranioplasty materials:
Biocompatibility: Titanium is famous for its uncommon biocompatibility. It has an interesting capacity to coordinate with human tissue without causing antagonistic responses. This property, known as osseointegration, permits titanium inserts to shape a solid bond with the encompassing bone, advancing long-term steadiness and decreasing the chance of embed dismissal.
Strength and Durability: Titanium gloats a noteworthy strength-to-weight proportion, making it both strong and lightweight. This characteristic is vital in cranioplasty, where the embed must withstand day by day stresses whereas not including superfluous weight to the patient's head. The toughness of titanium guarantees that the embed can give long-lasting security to the brain.
Corrosion Resistance: Unlike some other metals, titanium exhibits excellent resistance to corrosion. This property is vital in the harsh physiological environment of the human body, where implants are exposed to various bodily fluids. The corrosion resistance of titanium contributes to its longevity and reduces the risk of complications associated with material degradation.
Radiolucency: Titanium is relatively radiolucent, meaning it allows X-rays and other imaging techniques to pass through with minimal interference. This property is invaluable for post-operative monitoring and follow-up imaging studies, enabling doctors to assess the healing process and detect any potential issues without the implant obscuring the view.
Customizability: Advanced manufacturing techniques, such as 3D printing and computer-aided design, have made it possible to create highly customized titanium implants. These patient-specific implants can be tailored to match the exact contours of the skull defect, resulting in improved aesthetic outcomes and better functional results.
Thermal Conductivity: Titanium's low thermal conductivity helps maintain a stable temperature around the implant site. This property contributes to patient comfort and reduces the risk of temperature-related complications.
Inertness: Titanium is chemically inert, meaning it does not react with surrounding tissues or fluids in the body. This inertness contributes to its excellent biocompatibility and reduces the risk of allergic reactions or other adverse effects.
These exceptional properties have made titanium plate brain surgery a preferred choice for many neurosurgeons. The material's ability to provide a stable, long-lasting, and biocompatible solution for cranial reconstruction has significantly improved patient outcomes and quality of life.
Advancements in Titanium Plate Brain Surgery
The field of titanium plate brain surgery continues to evolve, with ongoing research and technological advancements pushing the boundaries of what's possible in cranioplasty. Some notable developments include:
3D-Printed Titanium Implants: The advent of 3D printing technology has revolutionized the production of titanium implants. This technique allows for the creation of highly detailed, patient-specific implants that perfectly match the contours of the skull defect. 3D-printed titanium implants offer improved aesthetic results and can be designed with intricate internal structures that promote better tissue integration.
Surface Modifications: Researchers are exploring various surface treatments for titanium implants to enhance their biological performance. Techniques such as plasma spraying, acid etching, and the application of bioactive coatings can improve osseointegration and promote faster healing.
Hybrid Materials: Some studies are investigating the potential of hybrid materials that combine titanium with other biocompatible substances. For example, titanium mesh scaffolds coated with hydroxyapatite or incorporated with growth factors are being developed to enhance bone regeneration and improve long-term outcomes.
Antimicrobial Properties: To address the risk of post-operative infections, researchers are developing titanium implants with antimicrobial properties. This can be achieved through surface modifications or the incorporation of antimicrobial agents into the implant material.
Smart Implants: The concept of "smart" titanium implants is gaining traction. These advanced implants could potentially incorporate sensors to monitor various physiological parameters, providing real-time data to healthcare providers and enabling early detection of complications.
Minimally Invasive Techniques: Advances in surgical techniques are allowing for less invasive placement of titanium implants. These approaches aim to reduce surgical trauma, shorten recovery times, and improve overall patient outcomes.
Whereas titanium plate brain surgery has demonstrated to be exceedingly successful, it's imperative to note that the choice of fabric for cranioplasty ought to be made on a case-by-case premise. Components such as the measure and area of the imperfection, the patient's age and by and large wellbeing, and the surgeon's ability all play a part in deciding the most appropriate approach. In a few cases, a combination of materials may be utilized to accomplish ideal comes about. For occurrence, a titanium work might be utilized in conjunction with bone cement or other manufactured materials to give both auxiliary bolster and corrective molding.
Conclusion
While various materials are available for cranioplasty, titanium plate brain surgery has emerged as a leading choice due to its unique combination of properties. Its biocompatibility, strength, durability, and customizability make it an excellent option for reconstructing cranial defects. As technology continues to advance, we can anticipate even more innovative applications of titanium in neurosurgery, further improving patient outcomes and quality of life.
For those interested in learning more about medical titanium products and their applications in cranioplasty and other surgical fields, don't hesitate to reach out to the experts at INT. You can contact them at export@tiint.com for more information on their range of high-quality medical titanium materials.










 2025-07-30 09:22:25
2025-07-30 09:22:25


_1752462620877.webp)

_1749191822714.webp)