The Science Behind Titanium Plates in Orthopedic Surgery
Titanium plate for bone has become ubiquitous in orthopedic surgery due to their unique properties. These medical devices are crafted from high-grade titanium alloys, typically Ti6Al4V ELI (Extra Low Interstitial), which is renowned for its biocompatibility and strength. The science behind using titanium for bone repair is rooted in its exceptional characteristics:
Biocompatibility: Titanium is highly biocompatible, meaning it can coexist harmoniously with human tissue without causing adverse reactions. This property is crucial for implants that will remain in the body for extended periods or even permanently. The human body's acceptance of titanium minimizes the risk of rejection or inflammation, which can be common with other materials.
Osseointegration: One of the most remarkable features of titanium is its ability to osseointegrate. This process involves the direct structural and functional connection between living bone tissue and the surface of the implant. Osseointegration allows the titanium plate to become, in essence, part of the bone structure, providing long-term stability and support.
Corrosion Resistance: The human body is a complex chemical environment, and inserts must withstand potential erosion. Titanium shapes a steady oxide layer on its surface when uncovered to oxygen, making it exceedingly safe to erosion from real liquids. This resistance guarantees the life span of the embed and anticipates the discharge of hurtful metal particles into the body.
Strength-to-Weight Ratio: Titanium boasts an impressive strength-to-weight ratio, offering robust support while remaining lightweight. This quality is particularly beneficial in orthopedic applications, as it allows for strong fixation without adding unnecessary bulk or weight to the affected area.
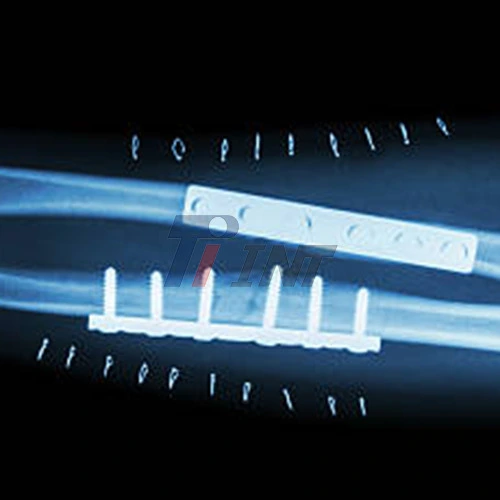
Radiolucency: Unlike some other metals used in medical implants, titanium is relatively radiolucent. This property allows X-rays and other imaging techniques to penetrate the implant, facilitating easier post-operative monitoring and assessment of the healing process.
Clinical Applications and Surgical Techniques
Titanium plate for bone repair find applications across a wide spectrum of orthopedic procedures. Their versatility allows surgeons to address various types of fractures and bone deformities effectively. Some common clinical applications include:
- Long Bone Fractures: Titanium plates are frequently used to treat fractures in long bones such as the femur, tibia, and humerus. These plates provide rigid fixation, allowing for early mobilization and rehabilitation.
- Facial and Cranial Surgeries: In maxillofacial and neurosurgery, titanium plates are used to reconstruct facial bones and secure skull fragments. The malleability of titanium allows surgeons to contour the plates to match the complex curves of the face and skull.
- Spinal Fusion: Titanium plates and rods are essential components in spinal fusion surgeries, providing stability to the vertebrae while fusion occurs.
- Joint Reconstruction: In procedures such as shoulder or elbow arthroplasty, titanium components play a crucial role in restoring joint function and stability.
The surgical techniques for implanting titanium plates have evolved significantly, with minimally invasive approaches gaining popularity. These techniques typically involve:
- Precise Preoperative Planning: Surgeons use advanced imaging and 3D modeling to plan the exact placement and configuration of titanium plates.
- Custom Plate Design: In some cases, titanium plates are custom-designed to fit a patient's specific anatomy, improving outcomes and reducing surgery time.
- Intraoperative Imaging: Real-time imaging during surgery ensures accurate placement of the titanium plate and screws.
- Minimally Invasive Insertion: Many procedures now use small incisions and specialized instruments to insert and secure titanium plates, reducing tissue damage and promoting faster recovery.
Patient Outcomes and Long-Term Considerations
The use of titanium plate for bone fracture repair has had a profound impact on patient outcomes. Studies have consistently shown improved healing rates, reduced complications, and enhanced quality of life for patients treated with titanium implants. Some key benefits include:
- Faster Recovery: The stability provided by titanium plates often allows for earlier weight-bearing and mobilization, accelerating the rehabilitation process.
- Reduced Risk of Infection: Titanium's biocompatibility and resistance to bacterial colonization contribute to lower infection rates compared to some other materials.
- Improved Fracture Healing: The rigid fixation provided by titanium plates creates an optimal environment for bone healing, often resulting in faster and more complete recovery.
- Long-Term Stability: Due to osseointegration, titanium plates provide long-lasting support, reducing the need for revision surgeries in many cases.
- Minimal Allergic Reactions: Titanium allergies are extremely rare, making it a safe choice for a wide range of patients.
Despite these advantages, there are some long-term considerations to keep in mind:
- Potential for Hardware Removal: In some cases, particularly in pediatric patients or those experiencing discomfort, titanium plates may need to be removed after the bone has healed.
- Stress Shielding: While rare with modern plate designs, there is a theoretical risk of stress shielding, where the bone may weaken due to the load-bearing properties of the plate.
- Metal Sensitivity: Although uncommon, some patients may develop sensitivity to titanium over time, necessitating removal of the implant.
- Imaging Artifacts: While titanium is more radiolucent than other metals, it can still create some artifacts in MRI and CT scans, potentially complicating future diagnostic imaging.
To mitigate these potential issues, ongoing research is focused on developing new titanium alloys and surface treatments to further enhance biocompatibility and reduce long-term complications.
Conclusion
The use of titanium plate for bone repair represents a pinnacle of medical engineering, combining cutting-edge materials science with advanced surgical techniques to deliver optimal patient care. As technology continues to advance, we can expect even greater innovations in this field, further cementing titanium's role as a cornerstone of orthopedic treatment.
For more information about medical titanium products, including titanium plates for bone repair, please contact Baoji INT Medical Titanium Co., Ltd. at export@tiint.com. With over 30 years of experience in the research, development, and production of titanium materials, INT is committed to providing high-quality, stable medical titanium materials to support the advancement of orthopedic care worldwide.










 2025-09-05 15:56:07
2025-09-05 15:56:07

_1750662309903.webp)






