Is it safe to implant a titanium plate in the brain?
 2025-12-25 09:17:04
2025-12-25 09:17:04
When it comes to brain surgery, the use of titanium plates has become progressively common. These medical wonders have revolutionized the field of neurosurgery, advertising hope and mending to patients with different neurological conditions. But an address that frequently emerges is: Is it safe to implant a titanium plate in the brain? Let's dive into this captivating point and investigate the security, benefits, and contemplations encompassing titanium plate for brain surgery.
|
|
|
Grasping Titanium Plates in Neurosurgery
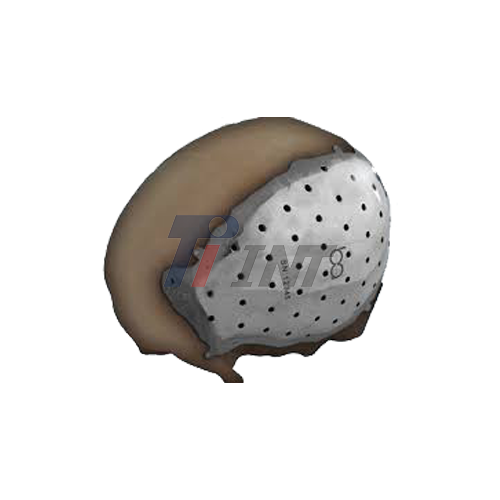
Titanium plates play a crucial part in brain surgery, serving as a protective shield and auxiliary back for the skull after certain strategies. These plates are ordinarily utilized in cranioplasty, a surgical strategy to repair cranial surrenders or anomalies. The utilization of titanium in restorative inserts has picked up ubiquity due to its unique properties, including biocompatibility, erosion resistance, and strength-to-weight proportion.
Neurosurgeons often select titanium plates when performing strategies such as tumor evacuations, treating traumatic brain wounds, or addressing congenital skull anomalies. The plates act as a substitute for the removed bone, giving assurance to the brain and reestablishing the skull's contour.
One of the key advantages of using titanium plates is their ability to integrate with the surrounding bone tissue. This process, known as osseointegration, ensures a stable and long-lasting fixation. Moreover, titanium's radiolucency allows for clear post-operative imaging, facilitating better monitoring and follow-up care.
Safety Considerations for Titanium Plate Implantation
The safety of implanting a titanium plate for brain surgery in the brain is a paramount concern for both patients and restorative experts. Broad research and clinical studies have been conducted to assess the security profile of titanium inserts in neurosurgery. The results have been overwhelmingly positive, with titanium plates illustrating fabulous biocompatibility and a low risk of unfavorable responses. One of the essential reasons for titanium's safety is its resistance to erosion. Not at all like some other metals, titanium does not corrode or discharge destructive particles into the encompassing tissue. This property essentially decreases the risk of irritation or dismissal by the body.
Furthermore, titanium plates are designed to be MRI-compatible, permitting patients to experience attractive reverberation imaging without concerns around the embedded interferometer with the results or causing harm. This compatibility is vital for continuous checking and potential future medicines.
While the overall safety profile of titanium plates is noteworthy, it's imperative to note that, as with any surgical procedure, there are potential dangers. These may incorporate contamination, bleeding, or complications related to the surgery itself. Be that as it may, these dangers are generally low and are not particular to the use of titanium plates. Neurosurgeons take great care in selecting appropriate candidates for titanium plate implantation. Factors such as the patient's overall health, the specific condition being treated, and the location of the implant are all carefully considered to ensure the best possible outcomes.
Advancements and Innovations in Titanium Plate Technology
The field of neurosurgery is constantly evolving, and so is the technology behind titanium plate for brain surgery. Recent advancements have focused on improving the design, manufacturing processes, and overall performance of these implants. One notable innovation is the development of patient-specific titanium plates. Using advanced imaging techniques and 3D printing technology, surgeons can now create custom-fit plates that perfectly match the patient's skull anatomy. This personalized approach enhances the aesthetic outcome and improves the functional results of the surgery.
Another area of advancement is in the surface treatment of titanium plates. Researchers have explored various coatings and modifications to enhance osseointegration and reduce the risk of infection. Some titanium plates now feature antimicrobial properties, further improving their safety profile. The integration of titanium plates with other materials, such as bioactive ceramics or polymers, is also being investigated. These composite implants aim to combine the strength of titanium with the bone-like properties of other materials, potentially improving long-term outcomes and reducing complications.
As technology continues to advance, we can expect to see even more sophisticated titanium plate for brain surgery designs and manufacturing techniques. These innovations will likely lead to improved safety, faster recovery times, and better overall results for patients undergoing brain surgery.
Conclusion
In conclusion, the implantation of titanium plates in the brain has proven to be a safe and effective approach in neurosurgery. The unique properties of titanium, combined with ongoing advancements in medical technology, have made these implants a valuable tool in treating various neurological conditions. While it's natural to have concerns about any surgical procedure, especially one involving the brain, the extensive research and clinical experience with titanium plates provide reassurance. The biocompatibility, durability, and safety profile of titanium make it an excellent choice for cranial implants.
As with any medical procedure, it's crucial for patients to have open discussions with their healthcare providers about the benefits, risks, and alternatives associated with titanium plate implantation. Each case is unique, and the decision to use a titanium plate should be made based on individual circumstances and expert medical advice. The field of neurosurgery continues to evolve, promising even safer and more effective treatments in the future. For those interested in learning more about titanium plate for brain surgery or other medical titanium products, please don't hesitate to reach out to experts in the field. You can contact us at export@tiint.com for more information on high-quality medical titanium materials and their applications in neurosurgery and beyond.
References
1. Wachter, D., Reineke, K., Behm, T., & Rohde, V. (2013). Cranioplasty with polymethylmethacrylate (PMMA) versus titanium: A randomized clinical trial. World Neurosurgery, 80(6), e307-e314.
2. Cabraja, M., Klein, M., & Lehmann, T. N. (2009). Long-term results following titanium cranioplasty of large skull defects. Neurosurgical Focus, 26(6), E10.
3. Pikis, S., Goldstein, J., & Spektor, S. (2015). Potential neurotoxic effects of polymethylmethacrylate during cranioplasty. Journal of Clinical Neuroscience, 22(1), 139-143.
4. Williams, L. R., Fan, K. F., & Bentley, R. P. (2015). Custom-made titanium cranioplasty: early and late complications of 151 cranioplasties and review of the literature. International Journal of Oral and Maxillofacial Surgery, 44(5), 599-608.
5. Kung, W. M., Chen, S. T., Lin, C. H., Lu, Y. M., Chen, T. H., & Lin, M. S. (2012). Verifying three-dimensional skull model reconstruction using cranial index of symmetry. PLoS One, 7(10), e48281.