Understanding Mandibular Fractures and the Role of Titanium Plates
The mandible, or lower jaw, plays a crucial role in various functions, including speech, mastication, and facial aesthetics. When a mandibular fracture occurs, it can significantly impair these functions and cause considerable discomfort. Titanium plates have become increasingly popular in mandibular fracture repair due to their exceptional strength-to-weight ratio, biocompatibility, and corrosion resistance.
Titanium plate for mandibular fracture repair are designed to provide stable fixation of bone fragments, allowing for proper healing and restoration of function. These plates come in various shapes and sizes, tailored to fit different anatomical regions of the mandible and accommodate diverse fracture patterns. The use of titanium in medical implants has revolutionized the field of orthopedics and maxillofacial surgery, offering patients a reliable and durable solution for fracture repair.
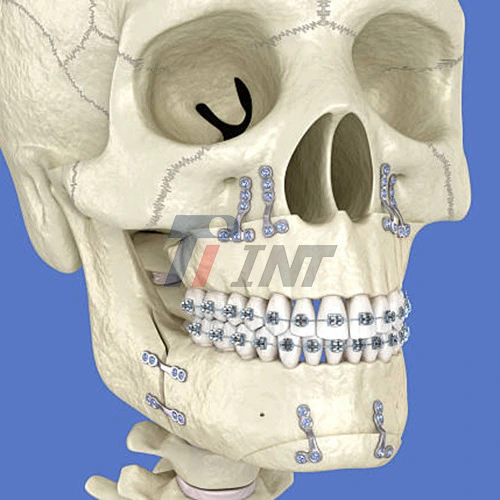
The process of mandibular fracture repair using titanium plates involves several key steps. Initially, the surgeon carefully assesses the fracture pattern and plans the placement of the titanium plates. The fractured bone segments are then accurately reduced and aligned. Subsequently, the titanium plates are contoured to match the mandibular anatomy and securely fixed to the bone using titanium screws. This rigid fixation ensures stability during the healing process, promoting optimal bone union and reducing the risk of malunion or nonunion.
Advantages of Titanium Plate Fixation in Mandibular Fracture Repair
The use of titanium plates in mandibular fracture repair offers numerous advantages over traditional wire fixation methods. These benefits contribute significantly to minimizing complications and improving overall patient outcomes:
- Enhanced Stability: Titanium plates provide superior stability to the fractured segments, allowing for early mobilization and faster recovery. This stability is particularly crucial in complex or comminuted fractures where maintaining proper alignment is challenging.
- Improved Healing: The rigid fixation provided by titanium plates promotes optimal bone healing by minimizing micro-movement at the fracture site. This environment fosters faster and more predictable bone union, reducing the risk of delayed healing or nonunion.
- Reduced Infection Risk: Titanium's biocompatibility and resistance to corrosion contribute to a lower risk of infection compared to other materials. The smooth surface of titanium plates also inhibits bacterial adhesion, further reducing the likelihood of postoperative infections.
- Minimized Soft Tissue Irritation: The low profile of modern titanium plates reduces soft tissue irritation and discomfort for patients. This design consideration is particularly beneficial in areas with thin overlying soft tissue, such as the mental region of the mandible.
- Versatility: Titanium plates can be easily contoured to match the unique anatomy of each patient's mandible. This adaptability allows for precise fixation in various fracture patterns and locations, including complex or multiple fractures.
- Long-term Stability: Unlike resorbable materials, titanium plates provide long-term stability without the risk of degradation over time. This characteristic is particularly advantageous in cases where prolonged support is necessary for optimal healing.
These advantages collectively contribute to a smoother recovery process, reduced complication rates, and improved patient satisfaction. The use of titanium plate for mandibular fracture repair has significantly enhanced the surgeon's ability to achieve predictable and favorable outcomes in even the most challenging cases.
Strategies for Minimizing Complications in Titanium Plate Fixation
While titanium plate fixation offers numerous benefits, it's essential to implement specific strategies to further minimize potential complications and optimize outcomes. Here are key considerations for surgeons and healthcare providers:
- Precise Preoperative Planning: Thorough preoperative assessment, including 3D imaging and virtual surgical planning, can significantly enhance the accuracy of plate placement and reduce operative time. This meticulous planning helps in selecting the appropriate plate size and configuration for each unique fracture pattern.
- Proper Plate Selection: Choosing the right titanium plate for mandibular fracture repair is crucial. Factors to consider include the location of the fracture, the degree of comminution, and the patient's bone quality. Using plates that are too rigid or too flexible can lead to suboptimal outcomes.
- Aseptic Technique: Maintaining strict aseptic conditions during surgery is paramount to prevent infection. This includes proper sterilization of instruments, use of antibiotic prophylaxis, and meticulous soft tissue handling.
- Accurate Fracture Reduction: Ensuring precise reduction of the fracture segments before plate fixation is essential for proper healing and restoration of occlusion. Intraoperative imaging can be valuable in confirming accurate reduction.
- Optimal Plate Positioning: Proper positioning of the titanium plate is crucial for stability and to avoid interference with tooth roots or neurovascular structures. The plate should be placed along the ideal line of osteosynthesis to counteract tensile and compressive forces.
- Appropriate Screw Selection: Using the correct screw length and diameter is essential to ensure secure fixation without damaging adjacent structures. Monocortical screws may be preferred in certain areas to avoid injury to tooth roots or nerves.
- Soft Tissue Management: Careful handling and closure of soft tissues over the titanium plate can prevent dehiscence and exposure. Tension-free closure and adequate soft tissue coverage are crucial for uneventful healing.
- Postoperative Care: Providing comprehensive postoperative instructions to patients, including oral hygiene measures and dietary restrictions, can significantly reduce the risk of complications. Regular follow-up appointments are essential to monitor healing progress and address any concerns promptly.
- Consideration of Patient Factors: Tailoring the treatment approach based on individual patient factors such as age, medical history, and lifestyle habits (e.g., smoking) can help mitigate potential complications. For instance, additional measures may be necessary for patients with compromised healing capacity.
By implementing these strategies, surgeons can harness the full potential of titanium plate fixation in mandibular fracture repair while minimizing the risk of complications. The synergy between advanced titanium plate technology and meticulous surgical technique results in optimal outcomes for patients suffering from mandibular fractures.
Conclusion
The use of titanium plate for mandibular fracture repair represents a significant advancement in maxillofacial surgery. By providing stable fixation, promoting optimal healing, and minimizing complications, titanium plate fixation has become the gold standard in mandibular fracture management. As technology and surgical techniques continue to evolve, we can anticipate even further improvements in patient outcomes and quality of life following mandibular fracture repair.
For more information on high-quality titanium products for medical applications, including titanium plates for mandibular fracture repair, please contact us at export@tiint.com. Our team of experts is dedicated to providing cutting-edge solutions that advance the field of medical implants and improve patient care.










 2025-12-17 08:34:05
2025-12-17 08:34:05
_1752820927376.webp)
_1752818317695.webp)
_1752462890412.webp)
_1752462199458.webp)