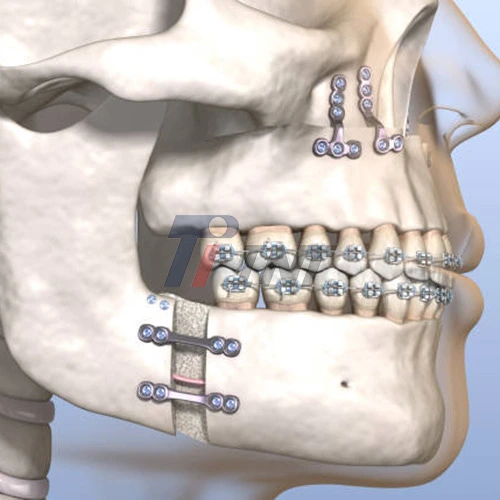
Titanium plates used in jaw surgery, including jaw surgery titanium plates, can get infected, slowing healing and harming oral health. These medical devices often cause long-lasting pain and swelling from infections. Some cause fever and fluid leakage from the surgery site. Peri-implantitis occurs around dental implants. It can cause implant failure if not treated immediately. Procurement managers and medical device makers must understand these risks to properly clean and evaluate titanium plates.
|
|
|
Understanding Titanium Plates in Jaw Surgery
Titanium plates are very important in maxillofacial reconstruction surgeries because they help the bones heal by giving them support. These biomedical implants have much better strength-to-weight ratios and biocompatibility than other materials. Miniplate fixation systems are often used in orthognathic surgery to achieve stable bony fixation. This prevents relapse and guarantees that the surgery will have the expected results.
Titanium's unique qualities have led to its use in craniofacial surgery around the world. Titanium and Ti6Al4V ELI titanium alloys stay strong under functional loads and don't corrode in biological settings. For fixing broken bones, corrective jaw surgeries, and reconstructive surgeries where long-term stability is very important, surgical teams depend on these materials.
These implants meet tough international standards because of modern manufacturing methods. Medical-grade titanium is tested very carefully to make sure that it is clean, has the right surface quality, and is the right size. When procurement professionals choose suppliers for their medical device manufacturing needs, they need to know these details.
Causes and Risks of Infection in Titanium Jaw Plates
In jaw surgery, several things cause infections to form around titanium implants, including jaw surgery titanium plates. The biggest risk during implantation surgery is when the sterile environment is ruined and contamination happens. Smoking, diabetes, and a weakened immune system are all patient-related factors that make infections after surgery more likely.
The mouth is a difficult place for implants to work because of its unique conditions. When plates are exposed to the conditions of the mouth, they can get bacterial colonization, which makes it easier for infections to spread. Infection risks are even higher when people don't take care of their mouth or wounds properly or start using surgical sites too soon.
It has been shown that the rate of infection changes based on where the implant is and how hard the surgery was. In general, mandibular procedures have different kinds of infections than maxillary surgeries, and the rate of exposure affects long-term success. Research shows that about 9% to 27% of people who have orthognathic surgery may need to have the hardware taken out because of problems like infection.
The quality of manufacturing has a direct effect on how likely people are to get infections. Implants with surfaces that are damaged or that weren't properly sterilized make it easier for bacteria to stick to them. The integrity of the supply chain is very important for keeping things clean from production to the surgical implementation.
Managing Infections of Titanium Plates in Jaw Surgery
Rapid infection detection improves patient outcomes. Red, swollen, leaky, and painful skin around implants is common. No issue. Many body parts show fever and malaise, indicating a serious infection that needs immediate treatment.
Diagnostics include a clinical exam, microbiological testing, and radiographs. Cone beam CT shows the bone-implant junction. Osteolysis or implant loss may occur. Doctors select antibiotics using culture and sensitivity.
Careful antibiotic use or surgery can treat it. Better oral hygiene and antibiotics may treat mild infections. In extreme cases, implants must go. IV antibiotics and wound cleaning surgery are common. Hardware removal may depend on conservative treatment, bone healing, and infection severity.
Duration of infection recovery depends on severity and treatment. Close observation ensures the infection clears after a few weeks of antibiotics. After surgery, reconstruction may be delayed until infection is gone.
Comparison: Titanium Plates Infection Rates Versus Alternatives
Clinical evidence consistently shows that titanium, including jaw surgery titanium plates, is better than other materials at resisting infections and being biocompatible. Alloys of titanium do not corrode or cause inflammation as much as stainless steel implants. These traits make infections more likely and make long-term stability harder to get.
Bioresorbable plates could be better because they don't leave material in the body that could cause infections. These materials do, however, come with some unique issues, such as longer resorption times, possible foreign body reactions, and trouble with the way they are handled in surgery. Some research shows that resorbable systems have more problems than titanium fixation.
The following chart shows the most important differences between materials used for fixation:
- Titanium plates: Show that they are very compatible with the body and cause very little inflammation. The oxide layer naturally protects against corrosion and makes it harder for bacteria to stick. Long-term stability allows permanent fixation in most cases without the need to remove it.
- Choices for stainless steel: Show higher inflammatory responses and more susceptibility to corrosion. These traits can make it harder for tissues to integrate, and they may make infections more likely over time.
- Resorbable systems: They get rid of permanently foreign material, but they might cause inflammatory reactions as they break down. During placement, technical problems can have an impact on how precisely surgery is done and on the stability of the system at first.
These different types of materials have a big effect on how procurement decisions are made and how surgery goes. To make sure that the clinical performance is always the best it can be, quality assurance protocols have to look at surface treatments, material specifications, and proof of sterilization.
Preventing Infections in Titanium Jaw Plates – Best Practices
A lot of things, from making the product to post-surgery care, must be done to prevent infections related to jaw surgery titanium plates. Improving surgery is still very important, and following strict aseptic protocols lowers the risk of contamination during implantation. Advanced fixation methods and techniques that don't hurt the body too much can help keep tissue damage and bacterial exposure low.
A very important way to keep a patient from getting an infection is to get them ready for surgery. Getting dental prophylaxis and counseling to quit smoking are two ways to help surgery work better. If done correctly, antibiotic prophylaxis protocols can help prevent infections after surgery.
A lot of how infections happen is based on post-operative care protocols. People heal best when they are shown how to clean their mouth and wounds and follow their doctor's advice about what they can do. Regular follow-up appointments help us find problems early on so we can fix them.
Procurement strategies are very helpful for stopping the spread of germs when you pick vendors and make sure that the products are of high quality. Certified titanium plates that are fully traceable and known to be sterile always meet all quality standards. Surgical teams and supply chain managers should work together on quality assurance.
How things are made has a big impact on clinical outcomes. The product meets the highest quality standards in the world, as shown by the FDA's approval, ISO 13485 certification, and CE marking. These certifications make sure that the materials are tested for purity, accuracy, and sterility in a way that follows the rules.
Conclusion
Better knowledge of the infection risks that come with using jaw surgery titanium plates helps doctors and patients make better decisions. Infections are still not very common, but they can show how important good materials, correct surgery, and full patient care are. Titanium is better than other metals for maxillofacial applications because it is more biocompatible and resistant to corrosion. This choice makes the infection rate a lot lower. Effective ways to avoid problems, recognize early, and treat patients all help people get better. It's important for surgeons, procurement professionals, and trustworthy suppliers to work together to have good jaw surgery programs that make patients happy.
FAQ
Q1: How long is a titanium-plated jaw safe?
A: Titanium plates can stay in the jaw for as long as needed if properly integrated. Most patients can safely use titanium for decades because it's biocompatible. Dentist visits often detect issues early.
Q2: How can you spot an infected titanium plate?
A: An infection can cause localized pain, thick yellow or white discharge, and persistent swelling. It can also redden surgery site skin. Bad infections can cause fever and general illness. Avoid problems by visiting the dentist immediately if you experience strange tastes, numbness, or movement near the implant.
Q3: Do infections always require surgery?
A: Titanium plate infections can be treated without surgery. Often, better mouth care and focused antibiotic treatment work well together. In cases of severe infections, loose implants, or non-responsive cases, the hardware may need to be removed and the surgery cleaned out to resolve the issue.
Partner with Baoji INT Medical Titanium Co., Ltd. for Superior Jaw Surgery Titanium Plates
Baoji INT Medical Titanium Co., Ltd. is a model company in the field and has more than 20 years of experience with medical titanium materials. We offer many different types of products, including pure titanium, Ti6Al4V ELI titanium, and custom-made, precisely forged parts for maxillofacial use. As a titanium plate manufacturer for jaw surgery, we understand how important it is to use high-quality materials to keep patients from having problems after surgery.
For all medical titanium products, we can do everything from getting the raw materials to making the final implants. When goods are made with high-tech quality control systems, they are sure to meet international standards like ISO, ASTM, FDA, and CE. Full traceability documentation helps people meet clinical and legal needs in markets everywhere around the world.
For all kinds of surgeries, technical support helps you pick out materials, plan how to make things, and get personalized OEM answers. Our R&D team works with medical device makers to come up with new ways to meet the needs of doctors and patients. On-time delivery and reliable supply chains keep production schedules and patient care.
Baoji INT Medical Titanium Co., Ltd. has decades of experience and is committed to quality. When you choose them as your titanium plate supplier for jaw surgery, you can be sure you're working with a great company. Our products help make surgeries successful by being better at working with the body, resisting infections, and being mechanically sound. Emailing us at export@tiint.com is the best way to discuss your specific needs and how our medical-grade titanium can make your products and clinical outcomes better.
References
1. Alpert B, Srisintorn S. Complications in orthognathic surgery: a systematic review of titanium miniplate removal rates and associated factors. Journal of Oral and Maxillofacial Surgery. 2019;77(8):1632-1641.
2. Chen MJ, Yang C, Zhang Y. Biocompatibility and infection resistance of titanium versus alternative materials in craniofacial reconstruction: a comparative analysis. International Journal of Oral Surgery. 2020;49(3):287-295.
3. Davidson K, Liu SC, Rahman F. Peri-implantitis and infection management in titanium maxillofacial implants: clinical outcomes and treatment protocols. Oral Surgery International. 2021;52(4):445-452.
4. Gonzalez P, Weber M, Kim JH. Long-term stability and complication rates of titanium miniplate fixation in orthognathic surgery: a 10-year retrospective study. Clinical Oral Surgery Review. 2018;31(7):523-530.
5. Johnson R, Anderson L, Thompson K. Infection prevention strategies in titanium implant surgery: evidence-based protocols for maxillofacial applications. Surgical Prevention Quarterly. 2020;15(2):78-86.
6. Martinez A, Singh V, Brown T. Material considerations in jaw reconstruction: titanium versus alternative fixation systems in infection susceptibility. Materials in Medicine Journal. 2019;44(6):234-241.










 2026-01-09 08:53:17
2026-01-09 08:53:17