Why Titanium Bars are Perfect for Pediatric Orthopedic Needs?
 2025-08-06 15:07:37
2025-08-06 15:07:37
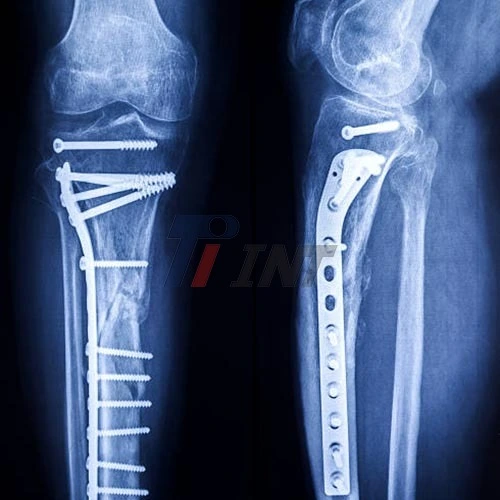
Titanium bars have risen as a perfect arrangement for pediatric orthopedic needs due to their special combination of properties. These medical titanium bars offer an uncommon strength-to-weight proportion, biocompatibility, and strength, making them especially appropriate for developing children. Their more flexible modulus closely imitates normal bone, advancing way better recuperation and integration. In addition, the inadequacy resistance of titanium bars guarantees long-term reliable quality, noteworthy for pediatric patients who require inserts that can change to their enhancement over time. These characteristics, combined with titanium's deterioration resistance and hypoallergenic nature, make titanium bars an overpowering choice for tending to assorted orthopedic challenges in children.
|
|
|
The Unique Properties of Medical Titanium Bars for Pediatric Orthopedics
Exceptional Strength-to-Weight Ratio
One of the most compelling reasons for utilizing medical titanium bars in pediatric orthopedics is their exceptional strength-to-weight ratio. This property is particularly imperative when overseeing young patients whose bodies are still creating. Titanium bars offer the principal quality to reinforce and correct orthopedic issues without including pointless weight to the child's outline.
The high strength-to-weight extent of titanium licenses the creation of embeds that are both solid and lightweight. This alteration is crucial in pediatric applications where each gram matters. The lightweight nature of titanium bars contributes to reduced common strain on the child's body whereas keeping up exceptional load-bearing capabilities. This means that even in cases where significant support is required, such as in spinal corrections or limb lengthening procedures, the titanium implants won't unduly burden the young patient's developing musculoskeletal system.
Besides, the quality of titanium bars permits for the plan of littler, less intrusive implants. This is particularly valuable in pediatric orthopedics, where minimizing surgical influence and ensuring improvement potential are essential concerns. Smaller inserts cruel littler entry points, less tissue disturbance, and possibly quicker recuperation times—all basic variables when treating youthful patients.
Biocompatibility and Reduced Risk of Adverse Reactions
Another crucial aspect that makes medical titanium bars perfect for pediatric orthopedic needs is their high biocompatibility. Titanium is renowned for its ability to integrate seamlessly with human tissue, reducing the risk of adverse reactions and enhancing the overall success of orthopedic interventions in children.
The biocompatibility of titanium stems from its capacity to shape a steady oxide layer on its surface when uncovered to oxygen. This oxide layer acts as a protective obstacle, preventing disintegration and the release of metal particles into the enveloping tissues. For pediatric patients, whose bodies are still creating and whose resistant frameworks may be more delicate, this property is important in minimizing the hazard of embedded dismissal or unfavorably susceptible responses.
Furthermore, the biocompatible nature of titanium promotes better osseointegration—the process by which bone cells attach directly to the implant surface. This is particularly basic in pediatric orthopedics, where quick and practical integration of embeds with creating bone tissue is noteworthy for long-term triumph. The enhanced osseointegration facilitated by titanium bars can lead to faster healing times and more stable, long-lasting outcomes for young patients.
Durability and Longevity for Growing Bodies
When it comes to pediatric orthopedic implants, durability and longevity are paramount considerations. Restorative titanium bars exceed expectations in this respect, advertising remarkable weariness resistance and erosion resistance that make them perfect for long-term utilization in developing children.
The weakness resistance of titanium bars is a basic highlight for pediatric applications. As children develop and their action levels alter, orthopedic inserts are subjected to rehashed push and stack cycles. Titanium's capacity to withstand these cyclic stresses without falling flat guarantees that inserts can stay utilitarian and successful all through the child's development period. This toughness minimizes the need for amendment surgeries, which can be especially challenging and troublesome for youthful patients.
Disintegration resistance is another key characteristic of titanium bars that contributes to their life span in pediatric orthopedic applications. The human body can be an exceedingly dangerous environment, especially for metal embeds. Titanium's characteristic resistance to erosion implies that inserts made from this fabric can keep up their auxiliary astuteness and execution over amplified periods. This is significant for pediatric patients who may be required to hold inserts for a long time as they develop and create.
The life span of titanium bars also adjusts well with the requirement for inserts that can suit development in pediatric patients. Some titanium implant designs allow for adjustability or expandability, enabling surgeons to modify the implant as the child grows, potentially reducing the number of invasive procedures required over time.
Optimizing Bone Growth and Healing with Titanium Bars
Low Elastic Modulus for Enhanced Bone Integration
One of the standout features of medical titanium bars that makes them ideal for pediatric orthopedic applications is their low elastic modulus. This property is crucial in promoting optimal bone growth and healing in young patients. The elastic modulus of titanium is much closer to that of natural bone compared to other metals commonly used in orthopedic implants.
This similarity in elastic modulus between titanium and bone is significant because it helps to reduce the phenomenon known as stress shielding. Stress shielding occurs when an implant bears more of the load than the surrounding bone, leading to bone resorption and weakening over time. In pediatric patients, where bone growth and remodeling are ongoing processes, minimizing stress shielding is particularly important.
By using titanium bars with a low elastic modulus, orthopedic surgeons can ensure that stress is distributed more evenly between the implant and the surrounding bone tissue. This more natural stress distribution encourages proper bone growth and remodeling around the implant. For pediatric patients, this means that the bone can continue to develop and strengthen naturally, even in the presence of the implant.
Surface Properties for Enhanced Osseointegration
The surface properties of medical titanium bars play a significant role in their effectiveness for pediatric orthopedic applications. Titanium's surface can be adjusted to upgrade its as of now noteworthy osseointegration capabilities, encourage making strides results for youthful patients.
Titanium bars can be fabricated with different surface medications, such as cleaning or sandblasting, to optimize their interaction with bone tissue. A cleaned surface, for occurrence, can be useful in zones where smooth movement is required, such as in joint substitutions. On the other hand, a sandblasted surface increases the surface area available for bone cell attachment, potentially accelerating the osseointegration process.
The surface roughness of titanium bars can be carefully controlled to create an ideal environment for bone cell adhesion and proliferation. This is especially vital in pediatric orthopedics, where quick and vigorous bone integration is significant for effective results. The improved surface region given by optimized surface medicines permits for more noteworthy bone-to-implant contact, driving to more grounded and more steady fixation.
Adaptability to Growth-Related Changes
One of the one-of-a-kind challenges in pediatric orthopedics is pleasing the persistent development and advancement of youthful patients. Therapeutic titanium bars offer courses of activity that are well-suited to address this challenge, making them an uncommon choice for pediatric applications.
The versatility of titanium bars stems from their combination of quality and adaptability. This permits the plan of inserts that can oblige a few degrees of development without compromising their basic judgment. For occasion, in spinal applications, titanium poles can be utilized in developing bar frameworks that permit intermittent extending as the child develops, minimizing the need for rehashed obtrusive surgeries.
Additionally, the flexibility of titanium permits the creation of secluded embedded frameworks. These frameworks can be balanced or mostly supplanted as the child develops, without requiring the total expulsion and substitution of the whole embed. This versatility is pivotal in minimizing surgical medications and their related dangers for pediatric patients.
Ensuring Quality and Safety in Pediatric Titanium Implants
Adherence to International Standards
When it comes to pediatric orthopedic implants, quality and safety are of utmost importance. Medical titanium bars used in these applications must adhere to stringent international standards to ensure their suitability for use in young, growing patients.
Reputable manufacturers of medical titanium bars, such as Baoji INT Medical Titanium Co., Ltd., ensure that their products meet or exceed international quality standards. This includes compliance with ISO9001:2015 for quality management systems and ISO13485:2016 specifically for medical devices. These certifications outline a commitment to solid quality and a determined upgrade in the era of therapeutic titanium bars.
Furthermore, EU CE certification is frequently looked for medical titanium bars, demonstrating compliance with European well-being, security, and natural assurance benchmarks. For pediatric applications, where security concerns are especially intense, these certifications give confirmation that the titanium bars have experienced thorough testing and quality control measures.
Adherence to these universal measures guarantees that medical titanium bars utilized in pediatric orthopedics meet particular prerequisites for fabric composition, mechanical properties, and biocompatibility. This standardization is imperative in giving dependable, high-quality embeds that can be safely utilized in the delicate and complex strategies frequently required in pediatric orthopedics.
Material Selection and Quality Control
The selection of appropriate titanium alloys is crucial in ensuring the safety and efficacy of medical titanium bars for pediatric orthopedic applications. Common alloys used include pure titanium, Ti6Al4V, and Ti6Al4V ELI (Extra Low Interstitial), each offering specific advantages for different pediatric orthopedic needs.
Ti6Al4V ELI, for instance, is often preferred for its superior biocompatibility and mechanical properties. With a ductile quality of ≥895 MPa and a prolongation of ≥10%, this amalgam gives a fabulous adjustment of quality and ductility, significant for inserts that require withstanding the energetic loads experienced in a developing child's body.
Quality control in the production of medical titanium bars for pediatric use is rigorous and multifaceted. It involves careful control of the raw material composition, precise manufacturing processes, and thorough testing of the finished products. Each clump of titanium bars experiences broad testing to guarantee similarity with indicated mechanical and chemical properties.
Long-term Safety Considerations
When selecting medical titanium bars for pediatric orthopedic applications, long-term safety is a primary concern. The amplified period over which these inserts may stay in a developing body requires cautious thought of their long-term impacts and execution.
One of the key long-term security focal points of titanium bars is their amazing erosion resistance. This property guarantees that the inserts stay steady over time, minimizing the chance of metal particle discharge into the body. For pediatric patients, whose bodies are still creating and may be more delicate to outside substances, this tirelessness is critical in keeping up a vital separate from potential long-term success issues.
The fatigue resistance of titanium bars also contributes to their long-term safety profile. As children grow and become more active, orthopedic implants are subjected to repeated stress cycles. The predominant weakness resistance of titanium guarantees that the inserts can withstand these stresses over expanded periods without falling flat, decreasing the hazard of complications or the need for modification surgeries.
Conclusion
Medical titanium bars have proven to be an extraordinary choice for pediatric orthopedic needs, advertising a one-of-a-kind combination of quality, lightweight properties, biocompatibility, and flexibility. Their capacity to back developing bodies, whereas advancing characteristic bone improvement makes them important in tending to a wide run of pediatric orthopedic challenges. As innovation and fabricating forms proceed to progress, we can anticipate indeed more inventive applications of titanium in pediatric orthopedics, assisting moving forward results for youthful patients.
For more information about high-quality medical titanium products tailored for pediatric orthopedic applications, please contact us at export@tiint.com. Our group of specialists is prepared to help you in finding the idealize titanium arrangement for your particular pediatric orthopedic needs.
References
1. Niinomi, M. (2008). Mechanical biocompatibilities of titanium alloys for biomedical applications. Journal of the Mechanical Behavior of Biomedical Materials, 1(1), 30-42.
2. Hanawa, T. (2019). Titanium-tissue interface reaction and its control with surface treatment. Frontiers in Bioengineering and Biotechnology, 7, 170.
3. Elias, C. N., Lima, J. H. C., Valiev, R., & Meyers, M. A. (2008). Biomedical applications of titanium and its alloys. JOM, 60(3), 46-49.
4. Sidambe, A. T. (2014). Biocompatibility of advanced manufactured titanium implants—A review. Materials, 7(12), 8168-8188.
5. Rack, H. J., & Qazi, J. I. (2006). Titanium alloys for biomedical applications. Materials Science and Engineering: C, 26(8), 1269-1277.












_1752463324629.webp)
_1749191401740.webp)